|
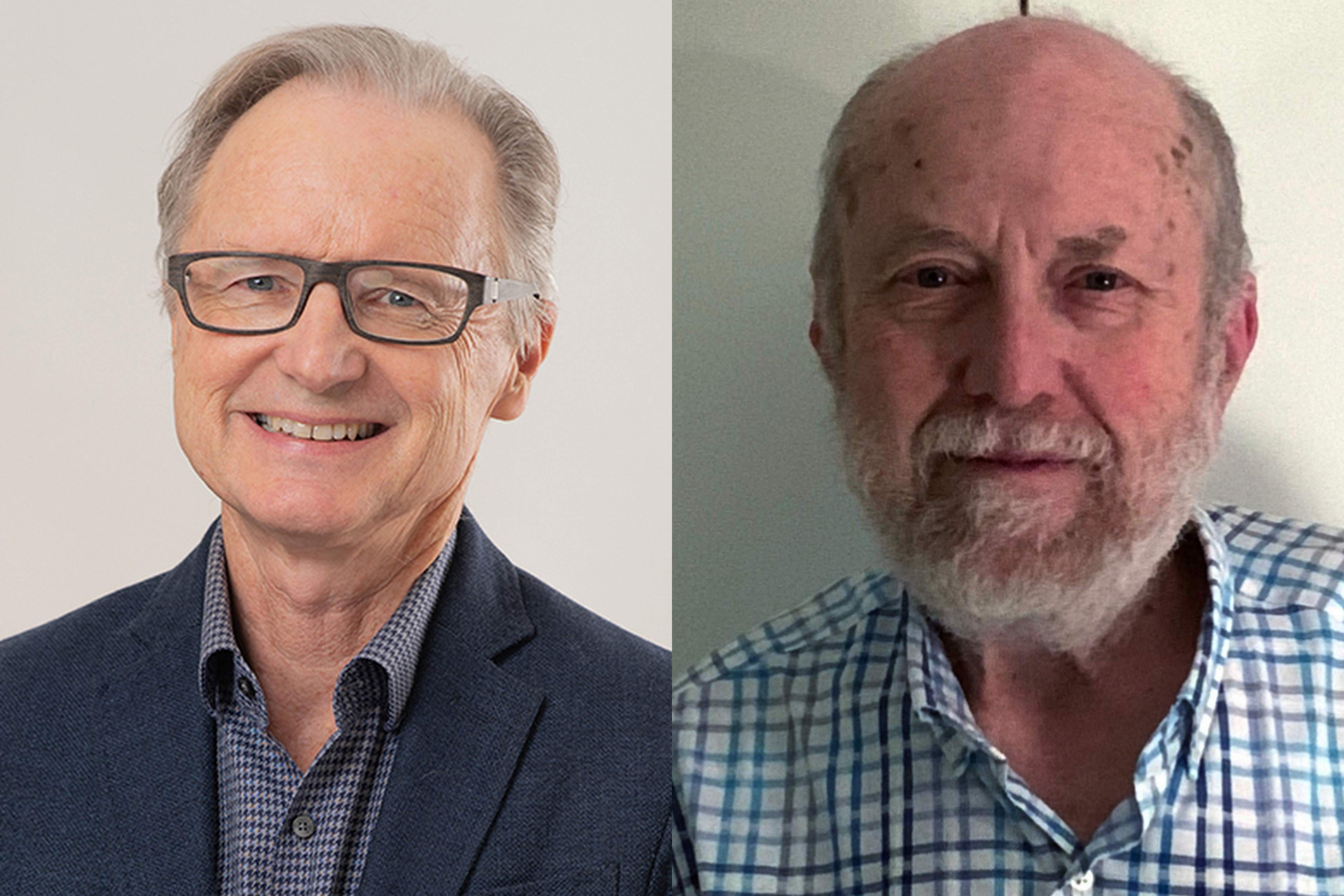
Panel of experts: Professor Timothy Hughes Professor Jeff Lipton |
Meet-the-CML-Expert Q&A Session on TKI Toxicities & Dose optimisation
Host: Stefanie Bockwinkel (iCMLf)
Links referred to in this session:
iCMLf Clinical Case Discussion Forum https://www.cml-foundation.org/science-education/case-discussions.html
iCMLf Knowledge Centre, Pediatric CML Module https://knowledge.cml-foundation.org/pediatric-cml/
Live questions during the presentation:
00:00 Welcome & Introduction
03:22 How do patients with ulcer manage the toxicity of TKI’s? It is really a big issue for some patients, if not all. TKI's are harsh, and not friendly with stomach issues like ulcers. It worsens ulcer issues for ulcer patients. What is your advice?
06:02 What can you say about phosphate levels and bone health in patients treated with TKI?
07:41 What are the long-term renal effects from imatinib, even at low doses of less than 400mg?
11:16 Do you see severe iron deficiency in patients treated with imatinib?
13:39 My biggest problem is cytopenia. There are patients who are unable to tolerate TKIs even when doses are reduced and different TKI used.
17:50 I am wondering if a person can become pre-diabetic while taking TKIs, especially bosutinib. Can the diagnosis be linked to TKIs, and if there is any history, is this more likely to be the cause?
21:20 It appears that each TKI drug has toxicity build-up over time. Given this, would it be prudent to have patients change TKI drugs every few years to avoid the build-up of specific toxicities, essentially "trading around" the toxicities to minimize overall impact?
27:30 Are there any recent studies regarding pediatric CML and how toxicity from TKIs can be monitored and administered?
29:09 Do you already start with doses lower than scheduled?
33:39 Do you reduce the dose upon reaching a milestone?
35:28 Do you think that reducing the dose before reaching a DMR would jeopardize reaching a subsequent DMR?
41:15 For ponatinib-induced drug rash, what should be the optimum dose of ponatinib in patients with blast crisis?
44:58 Does imatinib cause elevated thrombocytosis?
49:15 Thank you
Qustions answered following the live conversation:
Q1: Is it necessary to follow the serum levels in cases with non-optimal response and/or high toxicity?
We have conducted a lot of drug level studies and they do have clinical value but in the real world setting, the key to managing these challenging patients is in close molecular monitoring backed up with mutation screening and a readiness to move to another line of therapy if treatment failure has been established.
(Professor Timothy Hughes)
Q2: Would you consider alternating TKI dosage to manage toxicity while working towards DMR?
The first question that must be answered is whether the quest for DMR is worth the toxicity, given that even with CCyR, survival is virtually the same as DMR.
I am not sure what alternating the dosage means – dose one day alternating with a different dose the second day? Not sure that this will reduce toxicity. I would consider holding at a dose which is tolerable or consider a different drug. (Professor Jeff Lipton)
Q3: Diagnosed case of CML-CP can't tolerate 400/300 mg imatinib, but can tolerate 200 mg imatinib with haematological remission. Can we expect MMR of this type of cases by 200 mg imatinib daily?
Some people, especially of certain ethnicities, can possibly get deeper responses on 200 mg imatinib. I would expect that the majority of Caucasians at least would not get MMR on that dose.
Question that must be asked is what is the goal of therapy? CHR in an 80 year old may be all that you want. If this is a young person with hematological toxicity, then a consideration of an allograft may be in order. I would not be happy with just CHR in a young person. (Professor Jeff Lipton)
Q4: 300mg imatinib - elevated thrombocytes for the last 2 years. BCRABL1 is 0.0000. Reduce to 200mg? In DMR for 3 years.
If the patient is in a deep molecular response then the elevated platelet count is not due to the CML and another cause should be considered. Essential thrombocytosis and iron deficiency are two possibilities to JAK, CALr mutations and iron studies should be assessed. There is no need to reduce the imatinib dose since it would not be the cause of the thrombocytosis. (Professor Timothy Hughes)
Q5: Diagnosis on January 2023 with CML-AP due to additional chromosomal abnormalities per WHO guidelines. BCR-ABL at diagnosis was 60%. Started imatinib 400mg but at 3 months was at 30%. Started dasatinib 140mg 3 weeks ago but platelets is at 25. Platelets have been coming down from normal ever since imatinib started. What is your suggestion?
Thrombocytopenia and to a lesser extent neutropenia are two of the most challenging complications of TKI therapy. On going therapy will depend on whether there is an adequate molecular response to dasatinib. If the BCR::ABL1 level is less than 10% after 3 months of dasatinib then on going therapy at a dose of dasatinib that minimises cytopenia may be a good strategy. If dasatinib cannot be delivered because of severe cytopenia (grade 4) and/or no molecular response is achieved over the next 3-4 months, then an allograft may be the only strategy that will offer the prospect of a good long-term outcome. (Professor Timothy Hughes)
Q6: In your experience do you have any evidence of a link between possible renal effects of TKIs and kidney tumors?
People with CML are living long enough to get secondary cancers. Kidney cancer is the 6th most common type of cancer in the USA. There is no cause and effect data of any cancer and TKI therapy. All data is retroactive or registry and in one study, kidney cancer was ever so slightly higher than expected. No information on whether people getting kidney cancer have other risks or other kidney toxicity before they developed the kidney cancer. I have one case where a fire fighter got CML and kidney cancer within a few months of each other, but that is it. (Professor Jeff Lipton)
Q7: Though not yet published, we've observed differential pattern of TKI response among CML patients with specific cytokine gene polymorphism. I would be glad to hear your thoughts on this matter. With due respect and appreciation.
That’s an interesting observation. Anything is possible. Would like to see the data and then see if it can be duplicated in another data set. I am not sure what is meant by pattern of response. The response rate with TKIs is so good, is there enough of a difference to even look at this prospectively, i.e. determine the polymorphism at diagnosis and look at response curves. (Professor Jeff Lipton)
Please send any additional questions that you may have to info@cml-foundation.org.